An ocular migraine headache, also known as a visual migraine, is a type of migraine that primarily affects vision. Unlike typical migraines, which often involve severe headache pain, ocular migraines typically cause temporary visual disturbances without significant head pain. These disturbances can include:
-
- Aura: Visual disturbances such as flashing lights, zigzag lines, blind spots, or temporary loss of vision in one eye.
- Scotoma: A blind spot in the field of vision.
- Blurred vision: Difficulty focusing or seeing clearly.
These visual symptoms usually last for about 20 to 30 minutes and then resolve on their own. While ocular migraines are usually harmless and do not cause permanent vision loss, they can be alarming for those experiencing them.
Ocular migraine, also known as a visual migraine or a migraine with aura, is a type of migraine headache that is characterized by temporary visual disturbances or disruptions. These disturbances typically occur before or during the headache phase of a migraine attack and can affect one or both eyes. Ocular migraines are often associated with changes in blood flow, particularly in the blood vessels around or within the eye. The specific mechanisms are not fully understood, but these changes in blood flow are believed to contribute to the visual disturbances that characterize ocular migraines.

Symptoms
- Visual Aura: The hallmark of an ocular migraine is the visual aura, which can include various visual disturbances. Some common aura symptoms include:
- Flashing Lights: Bright, flickering lights that can resemble lightning bolts or stars.
- Zigzag Lines: Zigzag lines that move across the visual field in a jagged or shimmering pattern.
- Blind Spots (Scotomas): Temporary areas of reduced or lost vision in the field of view. These blind spots can vary in size and shape.
- Geometric Patterns: Visual disturbances may include the perception of geometric shapes or patterns.
- Blurry Vision: Vision may become blurry or distorted during the aura phase.
- Unilateral or Bilateral: Ocular migraines can affect vision in one eye (unilateral) or both eyes (bilateral). In some cases, the visual disturbances may start in one eye and then spread to the other.
- Temporary Duration: One key feature of ocular migraines is that the visual disturbances are usually short-lived, typically lasting for less than an hour. After the episode, normal vision usually returns.
- Headache (Optional): While not all individuals with ocular migraines experience headaches, some do. If a headache occurs, it often follows the visual aura and may be one-sided (unilateral), throbbing, and accompanied by other typical migraine symptoms such as nausea, vomiting, and sensitivity to light and sound.
- Other Neurological Symptoms (Rare): In some cases, ocular migraines can be associated with other neurological symptoms, such as tingling or numbness in the face or extremities. These symptoms are less common and may be indicative of a more complex migraine variant.
It’s essential to remember that ocular migraines are typically benign, and the visual disturbances are reversible. However, they can be quite unsettling and may cause anxiety. If you experience visual disturbances like those described above, especially if they are accompanied by severe headaches, it’s important to consult a healthcare professional for a proper diagnosis and to rule out other potential underlying medical conditions. Treatment for ocular migraines may involve medications to manage the symptoms and preventive measures to reduce the frequency and severity of future episodes.

Ocular Migraine Causes
The exact causes of ocular migraines, also known as migraines with aura, are not fully understood. However, they are believed to involve complex neurological and vascular mechanisms. Researchers have identified several factors and triggers that may contribute to the development of ocular migraines:
- Blood Flow Changes: Migraines, including ocular migraines, are thought to be related to changes in blood flow in the brain. It is believed that blood vessels in the brain may constrict (narrow) and then dilate (widen) during a migraine attack, which can lead to symptoms like visual disturbances.
- Cortical Spreading Depression: One theory is that ocular migraines are associated with a phenomenon called “cortical spreading depression.” This is a wave of abnormal electrical activity in the brain that can disrupt normal brain function, including vision.
- Genetics: There appears to be a genetic component to migraines, including ocular migraines. If you have a family history of migraines, you may be more prone to experiencing them yourself.
- Triggers: Ocular migraines, like other types of migraines, can be triggered by various factors. Common triggers include stress, hormonal changes (such as in women during their menstrual cycle), certain foods (e.g., aged cheeses, chocolate, and processed foods with additives), alcohol, caffeine, dehydration, lack of sleep, and changes in weather.
- Hormonal Changes: Hormonal fluctuations, such as those that occur during menstruation, pregnancy, or menopause, can influence migraine patterns in some individuals.
- Environmental Factors: Environmental factors, such as bright or flickering lights, strong odors, and loud noises, may trigger ocular migraines in susceptible individuals.
- Medications: Some medications, including certain vasodilators and hormonal therapies, may be associated with an increased risk of migraines, including ocular migraines, as a side effect.
Ocular Migraine Diagnosis
Diagnosing ocular migraines involves a comprehensive evaluation by a healthcare professional to rule out other possible causes of visual disturbances and to confirm that the symptoms are indeed related to migraines. Here are the steps typically involved in diagnosing ocular migraines:
- Medical History: Your healthcare provider will start by taking a detailed medical history. They will ask about your symptoms, including the nature and duration of visual disturbances, any associated headache, and any other accompanying symptoms. They will also inquire about your family history of migraines or other relevant medical conditions.
- Physical Examination: A physical examination will be conducted to rule out other medical conditions that may be causing your symptoms. This may include a neurological examination to assess your reflexes, coordination, and other neurological functions.
- Vision Testing: Your healthcare provider may perform a thorough eye examination to check for any underlying eye conditions that could be contributing to your symptoms.
- Diagnostic Criteria: To diagnose ocular migraines, your symptoms must meet specific diagnostic criteria established by medical guidelines. These criteria typically include the presence of visual disturbances (such as flashing lights or zigzag lines) that are fully reversible and accompanied by or followed by a headache. The visual disturbances should not be attributed to another medical condition.
- Additional Tests: In some cases, additional tests may be ordered to rule out other potential causes of visual disturbances. These tests may include blood tests, imaging studies (such as MRI or CT scans), and other diagnostic procedures.
- Patient History and Diary: Keeping a detailed diary of your symptoms, including when they occur, their duration, and any potential triggers, can be helpful in the diagnostic process. This information can provide valuable insights into the pattern and nature of your migraines.
- Discussion of Triggers: Your healthcare provider may discuss potential migraine triggers with you. Identifying and avoiding triggers can be an important part of managing ocular migraines.
- Discussion of Treatment Options: Once a diagnosis of ocular migraine is confirmed, your healthcare provider will discuss treatment options with you. Treatment may include medications to manage symptoms during an attack and preventive measures to reduce the frequency and severity of future episodes.
Ocular Migraine Treatment and Prevention
The treatment of ocular migraines involves managing the symptoms during an attack and, when necessary, implementing preventive strategies to reduce the frequency and severity of future episodes. Treatment approaches can vary based on the individual’s specific symptoms, medical history, and healthcare provider’s recommendations. Here are the common treatment strategies for ocular migraines:
1. During an Ocular Migraine Attack:
- Rest and Relaxation: Finding a quiet, darkened room and resting in a comfortable position can help alleviate the discomfort associated with an ocular migraine attack.
- Hydration: Dehydration can be a trigger for migraines, so drinking water or a hydrating beverage may be helpful.
- Medications: Over-the-counter pain relievers like ibuprofen or aspirin may help relieve mild to moderate headache pain during an attack. For more severe headaches, prescription migraine medications may be required.
- Medications for Nausea: If you experience nausea and vomiting during an attack, anti-nausea medications may be prescribed.
2. Preventive Measures:
- Identifying Triggers: Keep a migraine diary to identify potential triggers and make lifestyle adjustments to avoid them. Common triggers include stress, certain foods, alcohol, and lack of sleep.
- Lifestyle Modifications: Maintaining a regular sleep schedule, managing stress through relaxation techniques, and adopting a consistent exercise routine can help reduce the frequency of migraine attacks.
- Dietary Changes: Some individuals find relief by avoiding certain trigger foods, such as caffeine, chocolate, aged cheeses, and foods containing additives like monosodium glutamate (MSG).
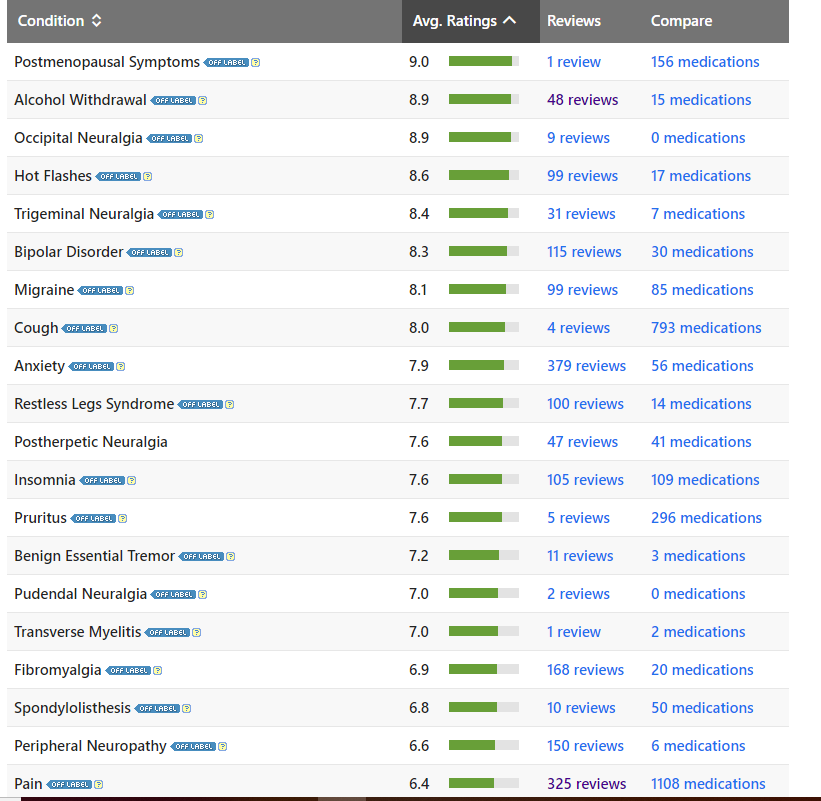
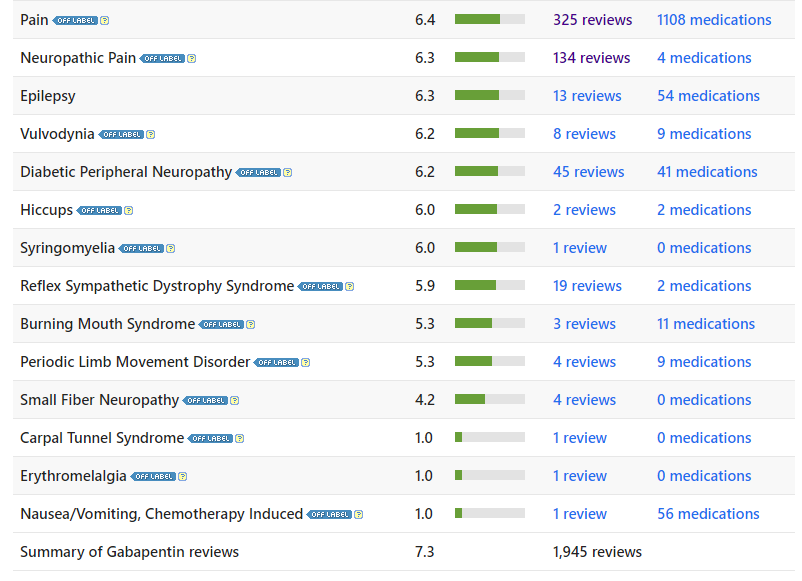
- Medications: Your healthcare provider may prescribe medications to prevent ocular migraines if they occur frequently, are severe, or significantly impact your quality of life. These medications can include beta-blockers, calcium channel blockers, anticonvulsants, tricyclic antidepressants, or newer migraine-specific drugs like calcitonin gene-related peptide (CGRP) inhibitors.
- Hormone Therapy: For individuals whose ocular migraines are hormonally triggered (e.g., menstrual migraines), hormone therapy or birth control methods may be considered.
- Vasodilators: In some cases, vasodilator medications may be prescribed to improve blood flow to the brain and reduce the risk of migraines.
- Botox Injections: Botox injections may be recommended for individuals with chronic migraines to prevent migraine episodes. This treatment is typically administered by a neurologist.
- Counseling or Cognitive Behavioral Therapy (CBT): Counseling or CBT can be helpful for managing stress and developing coping strategies for dealing with migraine triggers.
It’s essential to work closely with a healthcare provider to develop a personalized treatment plan tailored to your specific needs.