The largest group of over-the-counter painkillers are the non-steroidal anti-inflammatory drugs (NSAIDs). As their name suggests, they also reduce inflammation but – unlike other anti-inflammatory medicine – do not contain steroids. Over-the-counter NSAIDs are used in the treatment of many different kinds of pain, including headaches, period pain and toothache. NSAIDs reduce pain and inflammation and also lower fever.
There are more than ten different NSAIDs, but not all of them are available without a prescription or in every dose. In Germany and other countries, the following NSAIDs are available over the counter:
-
-
Acetylsalicylic acid (ASA, the drug in medicines like “Aspirin”) (in doses of up to 500 mg per tablet)
-
Diclofenac (up to 25 mg per tablet)
-
Ibuprofen (up to 400 mg per tablet)
-
Naproxen (up to 250 mg per tablet)
These medications are also by far the most commonly used NSAIDs.
Acetaminophen (paracetamol) is another very widely used painkiller. While also relieving pain and lowering fever, it doesn’t reduce inflammation (unlike NSAIDs).
In some medications it is combined with an NSAID (e.g. acetylsalicylic acid and acetaminophen). Caffeine is sometimes added too. It isn’t clear whether these kinds of combinations have any advantages or disadvantages over using the active ingredients separately. There are no good-quality studies comparing combination medications with individual drugs.
How do NSAIDs Work?
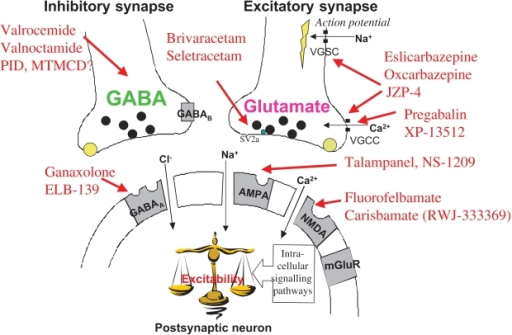
NSAIDs, or nonsteroidal anti-inflammatory drugs, work by inhibiting the activity of enzymes known as cyclooxygenases (COX enzymes). There are two main types of COX enzymes: COX-1 and COX-2.
- Inhibition of COX Enzymes: NSAIDs block the action of both COX-1 and COX-2 enzymes. These enzymes are involved in the production of prostaglandins, which are hormone-like substances that play a role in inflammation, pain, and fever.
- Reduction of Prostaglandin Production: By inhibiting COX enzymes, NSAIDs reduce the production of prostaglandins. Prostaglandins are responsible for promoting inflammation, sensitizing pain receptors, and causing fever. By decreasing prostaglandin levels, NSAIDs help alleviate pain, reduce inflammation, and lower fever.
- Anti-inflammatory Effects: NSAIDs exert anti-inflammatory effects by reducing the production of prostaglandins involved in the inflammatory response. This can help decrease swelling, redness, and heat associated with inflammation.
- Analgesic Effects: NSAIDs have analgesic (pain-relieving) properties by blocking the production of prostaglandins that sensitize pain receptors in the peripheral nervous system and spinal cord. This helps reduce the sensation of pain.
- Antipyretic Effects: NSAIDs also have antipyretic (fever-reducing) effects by inhibiting the production of prostaglandins involved in fever regulation in the brain’s hypothalamus.
It’s important to note that while NSAIDs are effective at reducing pain, inflammation, and fever, they can also have side effects, particularly when used at high doses or for prolonged periods. Common side effects of NSAIDs include gastrointestinal irritation, ulcers, bleeding, kidney problems, and an increased risk of cardiovascular events such as heart attack and stroke. Therefore, it’s essential to use NSAIDs as directed by a healthcare professional and to avoid exceeding the recommended dosage or duration of use.
What is the Right Dose of Pain Relievers?
The risk of side effects and complications can be reduced by using the lowest dose possible. It is generally important not to exceed the maximum single dose or the maximum daily dose. The information in the following table applies to Germany but may be very similar in other countries.
Table: Maximum daily dose for adults (without a prescription)
| Drug |
Maximum single dose |
Maximum daily dose |
| ASA |
1,000 mg |
3,000 mg in people under 65, 2,000 mg in people over 65 |
| Diclofenac |
25 mg |
75 mg |
| Ibuprofen |
400 mg |
1200 mg |
| Naproxen |
500 mg |
750 mg |
| Acetaminophen (paracetamol) |
1,000 mg |
4,000 mg |
Fixed-dose combination of acetylsalicylic acid
(ASA), acetaminophen and caffeine |
500 mg ASA / 400 mg acetaminophen/ 100 mg caffeine |
1,500 mg ASA / 1200 mg acetaminophen / 300 mg caffeine |
So if someone has a packet of 400 mg ibuprofen tablets, for instance, they should not take more than three tablets per day (24 hours).
Different NSAIDs shouldn’t be combined with each other. But an NSAID can be combined with acetaminophen if one medication alone isn’t effective enough.
Who has a particularly high risk of complications?
A number of personal factors increase the likelihood of NSAIDs causing problems. The risk of developing stomach or bowel problems is greater if you
-
-
are over the age of 65,
-
currently have a stomach ulcer or gastritis, or had one of them in the past,
-
have chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis),
-
take several NSAIDs at the same time,
-
are taking low-dose acetysalicylic acid (“Aspirin”) to prevent complications following a heart attack or stroke,
-
are taking anticoagulant (anti-clotting) medication, steroid medication or SSRI antidepressants.
NSAIDs also increase the risk of heart attacks or strokes, particularly in people who have already had one. These complications are more likely if you already have other kinds of cardiovascular disease or if you have risk factors such as high blood pressure.
In people who have decreased kidney function, taking NSAIDs can increase the risk of acute kidney failure. It is especially important for them to avoid taking too high a dose.
Which symptoms could be signs of complications?
Side effects like mild indigestion are not a cause for concern. But you should see a doctor if you have frequent or severe stomach pain, or if you notice signs of bleeding in the stomach. These include the following:
-
Black-colored stool (bowel movements)
-
Vomit with blood in it (red or black vomit)
-
Anemia symptoms such as exhaustion, shortness of breath during physical activity, or pale skin
In rare cases, ulcers can lead to perforation of the stomach wall (perforated ulcer). This complication is associated with sudden and very strong stomach pain. Perforation of the stomach wall is a life-threatening condition, so these symptoms should be taken seriously and the emergency services should be called immediately.
How can complications be prevented?
You can lower the risk of painkiller-related side effects and complications by paying attention to the package insert and
-
always taking “as little as possible, as much as necessary,”
-
only taking painkillers for as long as really needed,
-
watching out for possible interactions with other medications, and
-
checking whether certain painkillers aren’t suitable if you have any of the risks or medical conditions described above.
Which symptoms could be signs of complications of taking Pain Relievers ?
Side effects like mild indigestion are not a cause for concern. But you should see a doctor if you have frequent or severe stomach pain, or if you notice signs of bleeding in the stomach. These include the following:
-
Black-colored stool (bowel movements)
-
Vomit with blood in it (red or black vomit)
-
Anemia symptoms such as exhaustion, shortness of breath during physical activity, or pale skin
In rare cases, ulcers can lead to perforation of the stomach wall (perforated ulcer). This complication is associated with sudden and very strong stomach pain. Perforation of the stomach wall is a life-threatening condition, so these symptoms should be taken seriously and the emergency services should be called immediately.
Knowing the possible signs of a heart attack or stroke can also be helpful.